| Tauroursodeoxycholic acid Basic information |
| Overview Indication Mode of action Pharmacological effects Therapeutic applications of TUDCA References |
| Product Name: | Tauroursodeoxycholic acid |
| Synonyms: | yl)amino)-;Ursodeoxycholyltaurin;3α,7β-dihydroxy-5β-cholan-24-oic acid n-(2-sulfoethyl)amide;TUDCA Soduim Salt;TAUROURSODEOXYCHOLIC ACID DIHYDRATE: 90%;2-[[(3a,5,7)-3,7-Dihydroxy-24-oxocholan-24-yl]amino]ethanesulfonic Acid Sodium Salt;3a,7-Dihydroxy-5-cholan-24-oic Acid N-(2-Sulfoethyl)amide;Tauroursodeoxycholic acid sodium salt, 3α,7β-Dihydroxy-5β-cholan-24-oic acid N-(2-sulfoethyl)amide |
| CAS: | 14605-22-2 |
| MF: | C26H45NO6S |
| MW: | 499.7 |
| EINECS: | 1308068-626-2 |
| Product Categories: | Miscellaneous Natural Products;Bile Acids;Biochemistry;Steroids;Chiral Reagents;Inhibitors;Intermediates & Fine Chemicals;Pharmaceuticals;Herb extract;14605-22-2 |
| Mol File: | 14605-22-2.mol |
 |
| Tauroursodeoxycholic acid Chemical Properties |
| Melting point | 173-175°C |
| density | 1.216±0.06 g/cm3(Predicted) |
| refractive index | 46 ° (C=1, EtOH) |
| storage temp. | +15C to +30C |
| solubility | Soluble in DMSO (up to 30 mg/ml) or in Ethanol (up to 20 mg/ml with warming) |
| pka | 1.42±0.50(Predicted) |
| form | solid |
| color | White |
| Stability: | Stable for 1 year from date of purchase as supplied. Solutions in DMSO or ethanol may be stored at -20°C for up to 1 month. |
| InChIKey | BHTRKEVKTKCXOH-LBSADWJPSA-N |
| CAS DataBase Reference | 14605-22-2(CAS DataBase Reference) |
| Safety Information |
| Safety Statements | 22-24/25 |
| WGK Germany | 2 |
| RTECS | KI7372500 |
| HS Code | 29242990 |
| Toxicity | mouse,LD50,intravenous,350mg/kg (350mg/kg),Japanese Kokai Tokyo Koho Patents. Vol. #92-235918, |
| Tauroursodeoxycholic acid Usage And Synthesis |
| Overview | Tauroursodeoxycholic acid[TUDCA], the more hydrophilic form of ursodeoxycholic acid[UDCA], is the more abundant naturally produced bile acid in humans. Moreover, tauroursodeoxycholic acid is found in bears with high amount and has been used for centuries as a natural remedy in some Asian countries[1]. It has been approved in Italy and Turkey for the treatment of cholesterol gallstones and as well as being investigational drug in China, Unites States, and Italy. Tauroursodeoxycholic acid is also under investigation of its potential therapeutic effects on Primary Biliary Cirrhosis[PBC], insulin resistance, amyloidosis, Cystic Fibrosis, Cholestasis, and Amyotrophic Lateral Sclerosis. The only completed clinical trial thus far is a phase III clinical trial comparing tauroursodeoxycholic acid and ursofalk in PBC adult patients, but as of June 2013 no results of this trial have been published[1].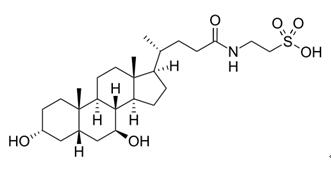 Figure 1 The chemical structure of TUDCA. Bear bile was historically employed to treat a number of diseases including jaundice, summer diarrhea, abdominal pain due to hepatobiliary diseases and gastric malfunction, biliary ascariasis, infectious skin diseases, the common cold, intestinal worms, and inflammation of the throat[2]. The principal bile acid that makes up bear bile is UDCA and its conjugates. UDCA and TUDCA make up 47 % of the biliary bile acid pool in the North American Black Bear, whereas in other vertebrates, are found in <5 % proportions[3]. Both TUDCA and UDCA circulate in plasma and comprise 28 % of circulating bile acids in bears and <1 % in humans[4, 5]. UDCA was first used as treatment of cholelithiasis in the 1970s[6]. In the 1980s and early 1990s, published studies concluded that treatment with UDCA might prove to be a safe and effective option for patients with primary biliary cirrhosis[7, 8]. Soon after, TUDCA was shown to protect against cholestasis and have greater cytoprotective effects along with decreased lithocholate formation compared to UDCA treatment[9, 10]. |
| Indication | It can be used in the treatment of cholesterol gallstones. Tauroursodeoxycholic acid is also being investigated for use in several conditions such as Primary Biliary Cirrhosis(PBC), insulin resistance, amyloidosis, Cystic Fibrosis, Cholestasis, and Amyotrophic Lateral Sclerosis[1]. |
| Mode of action | Tauroursodeoxycholic acid is the more hydrophilic form of ursodeoxycholic acid, which is naturally produced in the body. In patients with properly functioning gallbladders, both of these bile acids inhibit liver cholesterol secretion and synthesis as well as intestinal cholesterol absorption allowing for the promotion of cholesterol gallstone dissolution. The main mechanisms supporting possible Neuroprotective effects of TUDCA include the prevention of apoptosis. Specifically, TUDCA has been shown to inhibit apoptosis by modulating mitochondrial membrane perturbation and pore formation, B cell lymphoma 2[Bcl-2]-associated protein X(BAX) translocation, cytochrome c release, and caspase activation[11]. TUDCA inhibits amyloid beta[Ab]-induced apoptosis and attenuates the endoplasmic reticulum(ER) stress, which are thought to be key components of the pathological process in certain diseases[12,13]. |
| Pharmacological effects | TUDCA inhibits apoptosis Studies have shown that TUDCA is active in multiple steps of the apoptotic pathway. Apoptosis plays a crucial role in maintaining homeostasis, in physiological processes, and in many diseases[14]. TUDCA acts to inhibit apoptosis by modulating both the extrinsic and intrinsic pathways of apoptosis, activating cAMP response element-binding protein(CREB), and initiating cell survival pathways. In early studies of TUDCA and its cytoprotective effects, it was shown that TUDCA prevents release of cytochrome c, cytosolic caspase activation, and cleavage of the nuclear enzyme PARP to halt the apoptotic pathway[15]. In addition, a study published in 2000 showed that TUDCA prevents the depolarization of the mitochondrial membrane and the translocation of BAX from the cytosol[16]. TUDCA is equally effective at reducing p53-induced apoptosis and modulating the expression of Bcl-2[17]. P53 upregulates apoptotic proteins such as BAX and apoptotic protease-activating factor 1(Apaf-1), so by inhibiting p53 TUDCA can control the action of various other proteins involved in the mitochondrial pathway. TUDCA can also inhibit the action of caspase 2, 3, 6, and 9 either directly or indirectly helping to stop caspase-dependent apoptosis[18]. TUDCA modulates Amyloid-beta-induced apoptosis Aβ peptide is implicated in the pathogenesis of neurological diseases such as Alzheimer’s, where there is a loss of neuronal cells through the process of apoptosis[19]. Aβ causes significant induction of apoptosis in cortical neurons and is associated with a translocation of pro-apoptotic BAX to the mitochondria[20]. TUDCA modulates this event and the subsequent steps of cytochrome c release, caspase activation and DNA/Nuclear fragmentation. It also inhibits Aβ peptide-induced apoptosis via modulation of the PI3K signaling cascade and regulation of the E2F-1/ p53/BAX pathway[21]. Moreover, TUDCA counteracts Aβ-induced apoptosis through interaction with the mineralocorticoid receptor(MR), which is an inhibitor of apoptosis[22]. MR decreases p53 levels and changes the ratio of pro-relative to anti-apoptotic Bcl-2 members. TUDCA targets a region of MR ligand binding domain and dissociates the nuclear steroid receptor(NSR) from heat shock protein-90. From here, the TUDCA/NSR complex translocates to the nucleus and modulates NSR activity, where it reduces Aβ-induced apoptosis. TUDCA modulates ER stress The ER plays an important role in regulating cellular responses to stress[23]. The ER reads and integrates apoptotic signals and can initiate an ERS mediated pathway to apoptosis. Accumulation of unfolded proteins in the ER induces ERS. This accumulation of mis-folded proteins leads to the unfolded protein response(UPR), which can either cause the cell to undergo apoptosis or to fix the unfolded proteins and restore balance. TUDCA has been shown to inhibit ERS and block the UPR before it needs to be initiated. PERK[PKR[RNA-dependent kinase]-like ER kinase] is a part of the UPR[24]. TUDCA activates PERK which leads to the inactivation of eukaryotic translation initiation factor 2(EIF2). This causes a reduction in protein synthesis, halting aggregation of mis-folded proteins. Any proteins left over are degraded through autophagy. TUDCA modulates protein kinase C TUDCA is a significant calcium agonist and induces a sustained increase in free Ca2+ ions[25]. Inositol 1,4,5-triphosphate-sensitive calcium stores are modulated by TUDCA, causing a calcium influx across the plasma membrane via calcium ion channels[26]. Influx of calcium across the hepatocellular membrane via Ni-sensitive calcium channels and intracellular calcium oscillations plays a role in vesicular exocytosis. Protein kinase C(PKC) helps to control calcium influx and secretory events, as well as stimulating biliary exocytosis[27]. Translocation of PKC occurs by a calcium-dependent manner and binding of membrane phospholipid cofactors, such as phosphatidylserine(PS). In addition, activation of PKC occurs by binding of diacylglycerol to the Ca-PKC-PS complex. TUDCA activates membrane-associated PKC and increases its activity of reducing ischemic damage and increasing secretory events[26]. TUDCA’s effect on hepatocellular calcium with subsequent involvement in the activation of PKC shows that TUDCA activates complex patterns of signals in hepatocytes to increase apical membrane exocytosis. |
| Therapeutic applications of TUDCA | Myocardial Infarction TUDCA may prove to be an effective treatment in patients suffering from a heart attack. Rivard et al.[29] conducted a study on the effect of TUDCA following MI in rats. The authors tested whether administering TUDCA to rats prior to an MI would improve cardiac function. TUDCA was administered prior to ligation of the left anterior descending coronary artery. TUNEL and caspase-3 activity were assessed 24 h post-injury to detect apoptosis. TUNEL labeling showed a reduction in apoptotic cells, and caspase-3 activity was significantly reduced in rats given TUDCA prior to ischemic heart injury. At 4 weeks post-injury, TUDCA-administrated rats showed a significantly smaller infarct area in the myocardium compared to the control. The TUDCA group also showed improvement in shortening fraction assessed via ultrasound. The authors concluded that TUDCA could be a viable option for reducing apoptosis in MI. Hemorrhagic Stroke Intracerebral hemorrhage(ICH) is a serious injury with incidence of 24.6 cases per 100,000 person years(with 30-day and 1-year mortality rates of 40 and 54 %, respectively)[30]. Only 12–39 % of patients with ICH achieve long-term functional independence[30]. Recent work has shown that apoptosis is a major pathological process in ICH, and apoptotic-inhibiting therapies may provide a new approach to treatment. Caspase-3 levels are raised during ICH and DNA fragmentation occurs, both markers for apoptosis[31]. Researchers have hypothesized treatment of ICH with TUDCA since it is a potent apoptosis inhibitor. Rodrigues et al.[32] determined that TUDCA reduces apoptosis and protects neurons from acute hemorrhagic stroke in a rat model of ICH. TUDCA was administered 1 h before, 1 h after, or 3 h after the ICH onset. The authors showed that TUDCA administered at all time points in the study reduced lesion volumes at 2 days by as much as 50 % and apoptosis was decreased by 50 % in the perihematoma regions. Rotational symmetry, limb placement, and stepping ability, markers to assess neurobehavioral deficits were improved in the treated groups. TUDCA modulated Bcl-2 expression, activated the AKt-1/protein survival pathway, and induced BAD phosphorylation. Akt phosphorylates BAD and blocks BAD-induced death of primary neurons[33]. They concluded that TUDCA was promising in the treatment of hemorrhagic stroke due to its neuro-protective effects and safe clinical use. Ischemic Stroke During hypoxic ischemia, cell death occurs via apoptosis and necrosis. There is an overexpression of BAX in tissue following focal ischemia, indicating increased levels of apoptosis[34]. Caspase inhibitors have been shown to be neuro-protective in rat models of hypoxic-ischemic brain injury demonstrating a role of apoptosis in ischemia-related injuries[35]. Hypotheses behind this phenomenon are that damage created by ischemia induces apoptosis if ischemia is prolonged and necrosis occurs. Treatments inhibiting apoptosis could show promise in improving outcomes from ischemia-related diseases and others listed above[14]. In fact, Endres et al.[36] showed that inhibitors of apoptosis, specifically caspase inhibitors, reduce brain damage after middle cerebral artery occlusion. Other Neurological and Non-neurological Diseases Neuroprotective effects of TUDCA in preclinical studies of Huntington’s disease(HD) have shown to significantly reduce striatal neuropathology in the transgenic mice model of HD mouse[37]. TUDCA has also shown to suppress Aβ-induced apoptosis in multiple models of Alzheimer’s disease(AD). In Parkinson’s disease(PD), the loss of neurons is mainly mediated by apoptosis triggered by mitochondrial dysfunction and increase in reactive oxygen species(ROS). TUDCA was demonstrated to have a beneficial role in survival and function of nigral transplant in a rat model of PD[38] and also to partially rescue mitochondrial dysfunction in genetic PD models in Caenorhabditis elegans[39]. Recently, TUDCA has been shown to be safe and potentially effective in the treatment of Amyotrophic Lateral Sclerosis or ALS(Amyotrophic lateral sclerosis). |
| References | https://www.drugbank.ca/drugs/DB08834Wang DQ, Carey MC. Therapeutic uses of animal biles in traditional Chinese medicine: an ethnopharmacological, biophysical chemical and medicinal review. World J Gastroenterol. 2014;20(29]:9952–75.Hagey LR, Crombie DL, Espinosa E, Carey MC, Igimi H, Hofmann AF. Ursodeoxycholic acid in the Ursidae: biliary bile acids of bears, pandas, and related carnivores. J Lipid Res. 1993; 34(11]:1911–7.Bentayeb K, Batlle R, Sanchez C, Nerin C, Domeno C. Determination of bile acids in human serum by on-line restricted access material–ultra high-performance liquid chromatography–mass spectrometry. J Chromatogr B. 2008;869(1–2]:1–8.Sola S, Garshelis DL, Amaral JD, Noyce KV, Coy PL, Steer CJ, Iaizzo PA, Rodrigues CM. Plasma levels of ursodeoxycholic acid in black bears, Ursus americanus: seasonal changes. Comp Biochem Physiol Toxicol Pharmacol. 2006;143(2]:204–8.Maton PN, Murphy GM, Dowling RH. Ursodeoxycholic acid treatment of gallstones: dose–response study and possible mechanism of action. Lancet. 1977;2(8052–8053]:1297–301.Lotterer E, Stiehl A, Raedsch R, Foelsch UR, Bircher J. Ursodeoxycholic acid in primary biliary cirrhosis: no evidence for toxicity in the stages I to III. J Hepatol. 1990;10(3]:284–90.Poupon R, Chretien Y, Poupon RE, Ballet F, Calmus Y, Darnis F. Is ursodeoxycholic acid an effective treatment for primary biliary cirrhosis? Lancet. 1987;1(8537]:834–6.Nakai T, Katagiri K, Hoshino M, Hayakawa T, Ohiwa T. Microtubule-independent choleresis and anti-cholestatic action of tauroursodeoxycholate in colchicine-treated rat liver. Biochem J. 1992;288(Pt 2]:613–7.Rodrigues CM, Kren BT, Steer CJ, Setchell KD. Tauroursodeoxycholate increases rat liver ursodeoxycholate levels and limits lithocholate formation better than ursodeoxycholate. Gastroenterology. 1995;109(2]:564–72.Amaral JD, Viana RJ, Ramalho RM, Steer CJ, Rodrigues CM. Bile acids: regulation of apoptosis by ursodeoxycholic acid. J Lipid Res. 2009;50(9]:1721–34.Ermilov VV, Nesterova AA. b-amyloidopathy in the Pathogenesis of Age-Related Macular Degeneration in Correlation with Neurodegenerative Diseases. Adv Exp Med Biol. 2016; 854:119–25.Korsak M, Kozyreva T. Beta Amyloid Hallmarks: From Intrinsically Disordered Proteins to Alzheimer’s Disease. Adv Exp Med Biol. 2015;870:401–21.Elmore S. Apoptosis: a review of programmed cell death. Toxicol Pathol. 2007;35(4]:495–516.Benz C, Angermuller S, Tox U, Kloters-Plachky P, Riedel HD, Sauer P, Stremmel W, Stiehl A. Effect of tauroursodeoxycholic acid on bile-acid-induced apoptosis and cytolysis in rat hepatocytes. J Hepatol. 1998;28(1]:99–106.Rodrigues CM, Stieers CL, Keene CD, Ma X, Kren BT, Low WC, Steer CJ. Tauroursodeoxycholic acid partially prevents apoptosis induced by 3-nitropropionic acid: evidence for a mitochondrial pathway independent of the permeability transition. J Neurochem. 2000;75(6]:2368–79.Ramalho RM, Borralho PM, Castro RE, Sola S, Steer CJ, Rodrigues CM. Tauroursodeoxycholic acid modulates p53-mediated apoptosis in Alzheimer’s disease mutant neuroblastoma cells. J Neurochem. 2006;98(5]:1610–8.Ramalho RM, Viana RJ, Low WC, Steer CJ, Rodrigues CM. Bile acids and apoptosis modulation: an emerging role in experimental Alzheimer’s disease. Trends Mol Med. 2008;14(2]:54–62.Sola S, Castro RE, Laires PA, Steer CJ, Rodrigues CM. Tauroursodeoxycholic acid prevents amyloid-beta peptide-induced neuronal death via a phosphatidylinositol 3-kinase-dependent signaling pathway. Mol Med. 2003;9(9–12]:226–34.Viana RJ, Nunes AF, Castro RE, Ramalho RM, Meyerson J, Fossati S, Ghiso J, Rostagno A, Rodrigues CM. Tauroursodeoxycholic acid prevents E22Q Alzheimer’s Abeta toxicity in human cerebral endothelial cells. Cell Mol Life Sci. 2009;66(6]:1094–104Ramalho RM, Ribeiro PS, Sola S, Castro RE, Steer CJ, Rodrigues CM. Inhibition of the E2F-1/p53/Bax pathway by tauroursodeoxycholic acid in amyloid beta-peptide-induced apoptosis of PC12 cells. J Neurochem. 2004;90(3]:567–75.Sola S, Amaral JD, Borralho PM, Ramalho RM, Castro RE, Aranha MM, Steer CJ, Rodrigues CM. Functional modulation of nuclear steroid receptors by tauroursodeoxycholic acid reduces amyloid beta-peptide-induced apoptosis. Mol Endocrinol. 2006;20(10]:2292–303.Seyhun E, Malo A, Schafer C, Moskaluk CA, Hoffmann RT, Goke B, Kubisch CH. Tauroursodeoxycholic acid reduces endoplasmic reticulum stress, acinar cell damage, and systemic inflammation in acute pancreatitis. Am J Physiol Gastrointest Liver Physiol. 2011;301(5]:G773–82.Gani AR, Uppala JK, Ramaiah KV. Tauroursodeoxycholic acid prevents stress induced aggregation of proteins in vitro and promotes PERK activation in HepG2 cells. Arch Biochem Biophys. 2015;568:8–15.Beuers U, Nathanson MH, Isales CM, Boyer JL. Tauroursodeoxycholic acid stimulates hepatocellular exocytosis and mobilizes extracellular Ca++ mechanisms defective in cholestasis. J Clin Invest. 1993;92(6]:2984–93.Beuers U,ThrockmortonDC,AndersonMS, IsalesCM,ThaslerW, Kullak-UblickGA, Sauter G,KoebeHG, PaumgartnerG,Boyer JL. Tauroursodeoxycholic acid activates protein kinaseCin isolated rat hepatocytes. Gastroenterology. 1996;110(5]:1553–63.27. Baiocchi L, Tisone G, Russo MA, Longhi C, Palmieri G, Volpe A, Almerighi C, Telesca C, Carbone M, Toti L, et al.TUDCA prevents cholestasis and canalicular damage induced by ischemiareperfusion injury in the rat, modulating PKCalpha-ezrin pathway. Transpl Int. 2008;21(8]:792–800.29. Rivard AL, Steer CJ, Kren BT, Rodrigues CM, Castro RE, Bianco RW, Low WC. Administration of tauroursodeoxycholic acid[TUDCA] reduces apoptosis following myocardial infarction in rat. Am J Chin Med. 2007;35(2]:279–95.Chan S, Hemphill JC 3rd. Critical care management of Intracerebral hemorrhage. Crit Care Clin. 2014;30(4]:699–717.Gong C, Boulis N, Qian J, Turner DE, Hoff JT, Keep RF. Intracerebral hemorrhage-induced neuronal death. Neurosurgery. 2001;48(4]:875–82[discussion 882–873].Rodrigues CM, Sola S, Nan Z, Castro RE, Ribeiro PS, Low WC, Steer CJ. Tauroursodeoxycholic acid reduces apoptosis and protects against neurological injury after acute hemorrhagic stroke in rats. Proc Natl Acad Sci USA. 2003;100(10]:6087–92.Datta SR, Dudek H, Tao X, Masters S, Fu H, Gotoh Y, Greenberg ME. Akt phosphorylation of BAD couples survival signals to the cell-intrinsic death machinery. Cell. 1997;91(2]:231–41.Hochhauser E, Kivity S, Offen D, Maulik N, Otani H, Barhum Y, Pannet H, Shneyvays V, Shainberg A, Goldshtaub V, et al. Bax ablation protects against myocardial ischemia-reperfusion injury in transgenic mice. Am J Physiol Heart Circ Physiol. 2003;284(6]:H2351–9.Cheng Y, Deshmukh M, D’Costa A, Demaro JA, Gidday JM, Shah A, Sun Y, Jacquin MF, Johnson EM, Holtzman DM. Caspase inhibitor affords neuroprotection with delayed administration in a rat model of neonatal hypoxic-ischemic brain injury. J Clin Invest. 1998;101(9]:1992–9.Endres M, Namura S, Shimizu-Sasamata M, Waeber C, Zhang L, Gomez-Isla T, Hyman BT, Moskowitz MA. Attenuation of delayed neuronal death after mild focal ischemia in mice by inhibition of the caspase family. J Cereb Blood Flow Metab. 1998;18(3]:238–47.Keene CD, Rodrigues CM, Eich T, Chhabra MS, Steer CJ, Low WC. Tauroursodeoxycholic acid, a bile acid, is Neuroprotective in a transgenic animal model of Huntington’s disease. Proc Natl Acad Sci USA. 2002;99(16]:10671–6.Duan WM, Rodrigues CM, Zhao LR, Steer CJ, Low WC. Tauroursodeoxycholic acid improves the survival and function of nigral transplants in a rat model of Parkinson’s disease. Cell Transplant. 2002;11(3]:195–205.Ved R, Saha S, Westlund B, Perier C, Burnam L, Sluder A, Hoener M, Rodrigues CM, Alfonso A, Steer C, et al. Similar patterns of mitochondrial vulnerability and rescue induced by genetic modification of alpha-synuclein, parkin, and DJ-1 in Caenorhabditis elegans. J Biol Chem. 2005;280(52]:42655–68. |
| Description | Tauroursodeoxycholic acid (TUDCA) is a hydrophilic bile acid synthesized in hepatocytes by the conjugation of ursodeoxycholic acid (UDCA) with the amino acid taurine. UDCA, which is made by gut bacteria, is FDAapproved in the United States for the treatment of certain cholestatic liver diseases. Humans make TUDCA to some extent, but it is found in copious amounts in the bile of bears. TUDCA is a classic inhibitor of endoplasmic reticulum (ER) stress. Reduces ER stress and adipose tissue inflammation in a mouse model of high fat diet-induced obesity. Blocks ER stress-induced NLRP3 inflammasome activation and hepatocyte death. Attenuates amyloid precursor protein processing and amyloid-β deposition in APP/PS1 mouse model. |
| Chemical Properties | Tauroursodeoxycholic acid is an off-White Solid. It is an ambiphilic bile acid. It is mainly found in black bear bile, which is the signature active ingredient in bear bile. It has antispasmodic, anticonvulsant, anti-inflammatory and gallstone dissolving effects. |
| Uses | Tauroursodeoxycholic acid (TUDCA) is a water-soluble bile salt naturally occurring in the body. When bile salts reach the intestines, they can be metabolized by bacteria into ursodeoxycholic acid (UDCA). TUDCA is formed when taurine binds to UDCA. TUDCA is used to treat cholestasis, a condition in which bile fails to flow from the liver to the duodenum. TUDCA, UDCA, and other soluble bile salts can counteract the toxicity of regular bile acids when the latter are backed up in the liver. TUDCA is also used to treat cholesterol gallstones, dissolving them to a size in which they may be passed. |
| Definition | ChEBI: Tauroursodeoxycholic acid is a bile acid taurine conjugate derived from ursoodeoxycholic acid. It has a role as a human metabolite, an anti-inflammatory agent, a neuroprotective agent, an apoptosis inhibitor, a cardioprotective agent and a bone density conservation agent. It derives from an ursodeoxycholic acid. It is a conjugate acid of a tauroursodeoxycholate. |
| Side effects | TUDCA is safe and well-tolerated in patients with liver transplants, liver cirrhosis, and other diseases, but no clinical data exist for treatments longer than 1 year. There were no significant differences in adverse events between those receiving standard immunosuppressants versus those receiving bile acids in addition. Other trials in liver cirrhosis (up to 6 months) and ALS (1 year) have also reported that TUDCA is well-tolerated with diarrhea being the only side effect (Elia et al., 2016; Ma et al., 2016; Pan et al., 2013; Crosignani et al., 1996). Tauroursodeoxycholic-Acid-Cognitive-Vitality-For-Researchers |
| Mode of action | Tauroursodeoxycholic acid is a bile acid taurine conjugate derived from ursodeoxycholic acid. Bile acid is made by the liver and stored in the gallbladder and helps with digestion. It has a role as a human metabolite, an anti-inflammatory agent, a neuroprotective agent, an apoptosis inhibitor, a cardioprotective agent and a bone density conservation agent. TUDCA is found in small quantities in human bile but at a higher concentration in the bile of black bears, which is the signature active ingredient in bear bile. It demonstrates anti-apoptotic activity in rodent models of tauopathy, Huntington’s disease, ischemic brain injury, and retinal disorders. |
| References | 1) Xie?et al.?(2002),?Effects of tauroursodeoxycholic acid on endoplasmic reticulum stress-induced caspase-12 activation; Hepatology,?36?592 2) Chen?et al.?(2016),?Chemical chaperones reduce ER stress and adipose tissue inflammation in high fat diet-induced mouse model of obesity; Sci. Rep., 6?27486 3) Lebeaupin?et al. (2015),?ER stress induces NLRP3 inflammasome activation and hepatocyte death; Cell Death Dis.,?6?e1879 4) Nunes?et al.?(2012),?TUDCA, a bile acid, attenuates amyloid precursor protein processing and amyloid-β deposition in APP/PS1 mice; Mol. Neurobiol.?45?440 |
| Tauroursodeoxycholic acid Preparation Products And Raw materials |